Ask the Expert: Top 10 Questions IVF Patients Should Ask Their Provider

Preparing for IVF is a significant emotional and physical journey—and being informed can help ease the unknowns. Whether you’re starting stimulation medications or planning an embryo transfer, it’s essential to ask thoughtful, informed questions of your fertility team.
This guide outlines 10 key questions to bring to your IVF consult or cycle check-in, plus a downloadable prep checklist at the end.
1. What Protocol Will I Be On and Why?
Ask your provider:
“Which stimulation protocol are you recommending, and how is it tailored to my situation?”
Common IVF protocols include antagonist, long Lupron, or microdose flare, depending on factors such as ovarian reserve, age, AMH, AFC, and previous cycle responses. Individualized treatment is shown to improve outcomes and reduce the risk of ovarian hyperstimulation syndrome (OHSS) (ASRM Practice Committee, 2022).
2. What Are the Side Effects or Risks of the Medications?
Ask your provider:
“What physical or emotional side effects should I expect, and what symptoms would be considered an emergency?”
Most people experience bloating, mood swings, and fatigue. Serious risks include OHSS—especially in high responders. Early warning signs can include rapid weight gain, severe bloating, and shortness of breath (Sources: ACOG FAQ178, ASRM 2022).
3. How Many Monitoring Appointments Should I Expect?
Ask your provider:
“How often will I need bloodwork and ultrasounds, and how flexible is the scheduling?”
Expect approximately 5–7 visits during stimulation to monitor blood hormone levels and follicle growth by ultrasound. Visits tend to be less frequent in the beginning of treatment and more frequent as the growing eggs are closer to being ready for retrieval.These visits help determine the optimal timing for your trigger injection, which is the final medication to stimulate the eggs to become mature and ready for egg retrieval.
4. What Should I Know About Egg Retrieval Day?
Ask your provider:
“What should I expect on retrieval day in terms of sedation and recovery?”
Egg retrieval is typically an outpatient procedure performed under IV sedation. You should plan to take the day off and avoid strenuous activity for at least 24–48 hours afterward.
Note: You’ll need someone to drive you home. On this day, you cannot work or make important decisions that day due to the effects of the anesthesia medications.
5. Will I Be Doing ICSI — and Why?
Ask your provider:
“Will you use ICSI (Intracytoplasmic Sperm Injection), and what’s the reason in my case?”
ICSI is often recommended when there are sperm quality concerns, low fertilization in past cycles, or when using frozen eggs or sperm. It may improve fertilization rates but does not necessarily improve live birth rates in cases without male-factor infertility (Source: ASRM Committee Opinion, 2020).
6. How Will Embryos Be Cultured and Graded?
Ask your provider:
“Can you explain your embryo grading process and how you decide which to transfer or freeze?”
Ask about the lab’s criteria for evaluating embryos on day 3 vs. day 5 (blastocyst stage), how grading influences selection, and what to expect in terms of embryo quality. Remember: even embryos with ideal grading aren’t guaranteed to implant, and lower-graded embryos may still result in pregnancy.
7. Will I Have a Fresh or Frozen Embryo Transfer?
Ask your provider:
“How do you decide between fresh and frozen embryo transfer in my case?”
Fresh transfers may be appropriate if hormone levels and uterine lining conditions are optimal. Frozen transfers are increasingly preferred for better timing and to reduce the risk of OHSS. ASRM supports both approaches based on individual factors (ASRM, 2022).
8. What Is the Ideal Lining Thickness for Transfer?
Ask your provider:
"What uterine lining thickness are you aiming for, and how do you support implantation?”
A lining between 7–12mm with a trilaminar appearance is often ideal. Hormonal support such as estrogen, progesterone, or medications to improve blood flow may be recommended.
9. What Should I Avoid After Retrieval and During the Two-Week Wait?
Ask your provider:
“What should I avoid in terms of exercise, travel, or other activities after retrieval and transfer?”
Most clinics recommend:
- Avoiding sex or high-impact exercise for 5–7 days post-retrieval
- Engaging in only light activity during the luteal phase or after transfer
- Avoiding alcohol, hot baths, and other activities that raise core body temperature
(Guidelines based on ACOG and ASRM, 2022)
10. What Are the realistic chances of pregnancy from IVF?
Ask your provider:
“What is the likelihood of pregnancy with IVF?”
It’s important to understand that:
- Even under ideal conditions, top-quality embryos implant only 50–60% of the time.
- Many people require multiple IVF or embryo transfer cycles before achieving a pregnancy.
- Discuss what defines success and when it might be appropriate to reconsider or stop treatment, based on both medical and emotional factors.
You should also talk to your care team about:
- Adjusting expectations and preparing for a potentially longer journey than initially hoped.
- How outcomes from this cycle will inform decisions about future protocols or testing.
- Support resources such as mental health counseling or peer support groups to help navigate the ups and downs of treatment.
Clinics should offer evidence-based guidance, not unproven interventions, and should help you make informed decisions grounded in realistic success rates and long-term well-being.
IVF Consultation Prep Checklist
Topics to discuss at your consult or check-in:
Medications & Protocol
- What stimulation protocol is being used?
- What side effects or emergency signs should I watch for?
- Should I stop any current medications or supplements?
Lab & Fertilization
- Will ICSI be used, and why?
- How are embryos graded and selected?
- What is the lab’s blastocyst development rate?
Cycle Logistics
- How many monitoring visits are required?
- What happens after my eggs are retrieved?
- Will I be doing a fresh or frozen transfer?
Lifestyle & Recovery
- Can I exercise or travel post-procedure?
- Are there any dietary or lifestyle recommendations for treatment?
- When can I resume sexual activity or high-impact movement?
Emotional & Contingency Planning
- What are the next steps if fertilization or implantation is unsuccessful?
- Are counseling or mental health services available?
Final Thoughts
IVF is more than a protocol—it’s a partnership. Asking the right questions helps ensure your care is personalized, evidence-based, and aligned with your values and goals.
Read more on our blog: Top 10 IVF Questions to Ask Your Provider
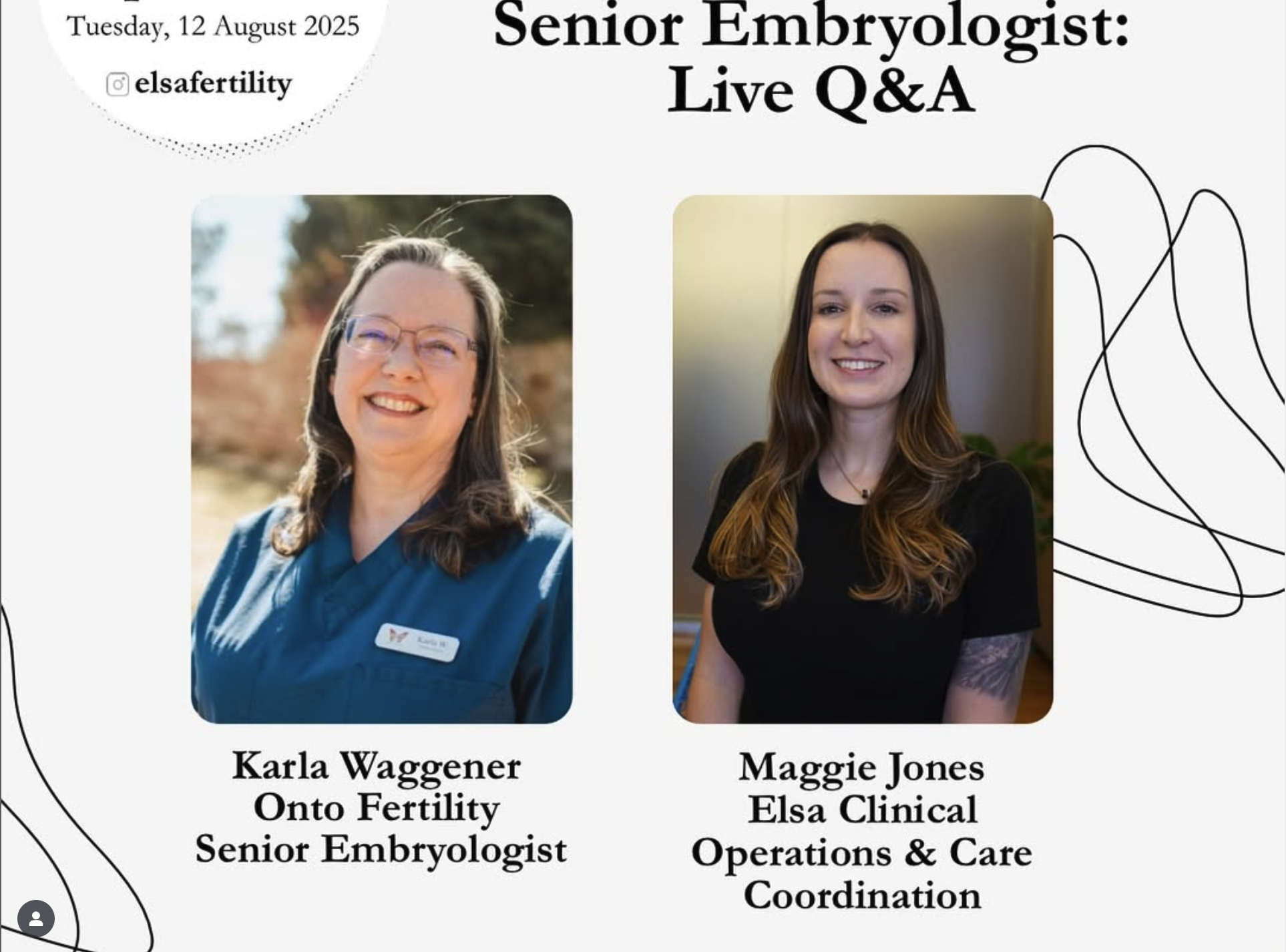
Elsa Fertility is here to support you every step of the way. Our care team is committed to helping you ask the right questions and make confident, informed decisions throughout your fertility journey.
Sources:
- ASRM Practice Committee. "Individualized ovarian stimulation protocols." Fertil Steril. 2022.
- ACOG. FAQ178: "Egg Freezing and Fertility Preservation."
- ASRM Committee Opinion: "ICSI for non-male factor infertility." 2020.
- ASRM Guidance on Elective Add-ons. 2021.
Articles Recommended for You
Modern, personalized, effortless
Join our mailing list to stay informed with the latest in fertility.